Promoting Oral Health Awareness in Dental Practices On March 20, 2026, dental healthcare professionals across…
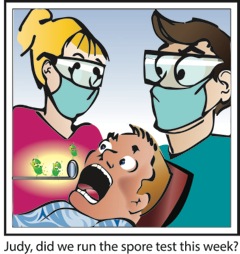
Sterilizer Monitoring Considerations
Monitoring of sterilization procedures includes a combination of process parameters to evaluate the sterilizing conditions and the procedures’ effectiveness. Regular sterilizer monitoring using biologic indicators has become the standard practice, and when properly implemented, is an important part of infection control verification.
Both the Centers for Disease Control and Prevention (CDC) and the American Dental Association recommend, and most state dental boards require, that dental offices verify the proper functioning of the sterilization cycle at least weekly using a biological indicator, such as the Spore Check System from OSHA Review, Inc. When spores are killed during a sterilization cycle, it is assumed that all microorganisms have been destroyed and sterilization is achieved.
How should I conduct the spore testing?
Biological indicators consist of highly resistant, nonpathogenic bacterial spores. Specific spores, Geobacillus stearothermophilus for steam/chemical sterilizers and Bacillus atrophaeus for dry heat sterilizers, are inoculated onto strips of specialized filter paper that is packaged in a peel open glassine paper pouch. Glassine paper is permeable to sterilant but resistant to moisture and air at ambient temperature/pressure. This allows the tester to transport the strip within the glassine from the sterilizer to the processing area, where it can be properly handled. Lot number and expiration date are printed on each glassine.
The glassine-bound spore strips should be placed according to the sterilizer manufacturer’s instructions. If there are no instructions, place the spore test strip within a wrapped set of instruments in the most difficult area to be sterilized, which is normally the lower front area of the sterilizer. It is good practice to place the strips in a different location of the sterilizer each week to help identify any “cold spots” within the sterilizer.
All staff members who operate the sterilizer should receive training about proper sterilizer operation procedures and instrument processing techniques in the office. Additionally, general sterilizer maintenance consisting of regular cleaning and checking of door gaskets, vents, and internal and external surfaces of the sterilizer should be conducted in accord with the sterilizer manufacturer’s instructions.
Are process indicators useful?
Process indicators such as autoclave tape are recommended within each load to show that certain physical parameters have been met within the sterilizer. They designate that a package has been placed through a sterilization cycle. They do not, however, prove that sterilization has occurred.
What if we receive a positive test?
Common factors for sterilization failures include chamber overload, excessive packaging material, inadequate exposure time, incorrect temperature/pressure settings, failure to preheat the sterilizer (if indicated), interruption of the sterilization cycle, and expired chemical solution (chemiclaves only).
If a process indicator turns positive, then retest with the process indicator immediately. Ensure that the process indicator has not expired and that the testing protocol has been met. Also check the sterilizer for any obvious inconsistencies.
In general, a single positive spore test probably does not indicate sterilizer malfunction, especially if the process indicators demonstrate sterilizer effectiveness. However, if you receive a positive spore test, contact your biological monitoring service immediately for assistance.
In Conclusion
Understanding and correctly implementing the factors that lead to successful sterilization results in a significant achievement toward an overall effective dental infection control program.
The Spore Check System is a weekly spore testing service brought to you by OSHA Review, Inc. For information about the Spore Check System, call 800-555-6248.